Survey: 1 in 4 healthcare organizations experience as much as $1 million annually in lost billings due to credentialing
While most respondents expressed confidence in their process, the contrast with the financial impact suggests a ‘credentialing confidence paradox’
The process lacks national standards, is hampered by manual processes, it delays a provider’s ability to deliver needed services – and by extension their employer's ability to generate revenue.”
WILLIAMSBURG, VA, UNITED STATES, January 15, 2026 /EINPresswire.com/ -- The process of credentialing healthcare providers after they’ve accepted a job offer is having a financial impact on healthcare organizations, according to a new survey by Intelliworx. — Intelliworx CEO Rob Hankey
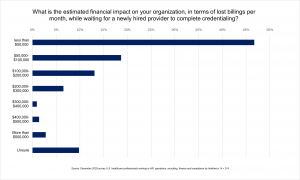
The survey polled 214 human resources, operations and finance professionals working for U.S. healthcare organizations. It found that more than four in 10 respondents said their healthcare organization experiences up to $50,000 in lost billings every month.
Another 25% say they miss out on billings to the tune of $100,000 a month or more. Further, one in 10 respondents reported lost billings in excess of $200,000 per month. On an annual basis, missed monthly billings can add up to millions of dollars in lost annual revenue.
“Healthcare is unique because after they’ve gone through the process of hiring a provider, which can easily take 3-4 months, they still have to finish the credentialing process before that provider can see patients and bill for services,” said Intelliworx CEO Rob Hankey. “The process lacks national standards, is hampered by manual processes, it delays a provider’s ability to deliver needed services – and by extension their employer's ability to generate revenue.”
Credentialing confidence paradox
The financial impact contrasts with the expressed confidence most respondents had about their credentialing processes. For example, 60% of respondents said they were "completely confident" that providers employed by their organization have up-to-date credentials. Another 31% are “fairly confident” that all credentials are current.
The survey also revealed that credentialing seems to be getting done faster, compared to historical benchmarks. More than eight in 10 said credentialing a provider takes 60 days or less. This includes 43% who said they get credentialing completed in 30 or fewer days.
This was a surprising finding, given that other surveys, conducted in prior years, indicated this process took anywhere from three to six months on average. The confidence and relative speed of credentialing reported by respondents seem to conflict with the financial impact of lost billings.
“The apparent contradiction between confidence in credentialing and the financial impact that this survey found suggests this may be a blind spot for healthcare leaders,” added Hankey. “It’s also an opportunity to improve efficiency, because respondents indicated the credentialing process is a prime candidate for improvement through automation.”
Credentialing is still a manual process
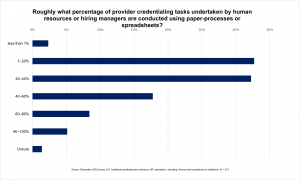
Many healthcare processes still rely on paper, spreadsheets and are largely manual. For example, it’s not uncommon to see fax machines still used for signatures, doctors’ orders and prescriptions. Credentialing, too, is reportedly a process where significant portions are still completed by hand.
For example, the survey found 64% of respondents say 20% or more of credentialing tasks are done by hand. Another 31% of respondents put that number at 40% or higher. Finally, another 13% say their credentialing process is more than 60% manual.
In open-ended remarks, many respondents seemed to acknowledge the shortcomings and expressed a desire for better automation. When asked what they would improve about their credentialing process, many wrote in proposing technological solutions.
“Automation with notifications of [credentialing] expiration,” wrote one respondent. “Communication [integration] between job boards and ATS [applicant tracking system],” said another. “I’d like for things to go through faster, AI is helping a lot,” a third respondent noted. “I hope that we get a good balance of AI with human oversight.”
Results of the survey are freely available online – no registration required – Lost billings: The financial impact of provider credentialing process in healthcare.
About the survey
Intelliworx polled 214 respondents using a commercially available survey panel from December 1, 2025, until December 9, 2025.
All respondents work for a U.S.-based healthcare organization and work for business functions including human resources (49%), business operations (20%), healthcare recruiting (16%), training & development (7%), finance or accounting (4%) and lastly, compliance or credentialing (3%).
Respondents also appear to be fairly experienced, with 86% indicating they have five or more years of experience. Further, nearly half (45%) said they have 10 years of experience in their role.
# # #
About Intelliworx
Intelliworx (formerly HRWorx, LLC) provides workflow management software that helps customers automate business processes such as financial disclosure, telework, credentialing, onboarding, and workflow, among others. The company got started 20 years ago by converting complex forms into intelligent interviews – similar to the way tax software simplified tax filing for consumers. Today, it’s evolved from a simple tool for data collection to a platform that supports entire processes of IT modernization and improves the customer experience (CX).
Intelliworx develops technology solutions for the U.S. Government, state and local governments and rural private sector healthcare facilities. It has provided purpose-built software to federal government agencies and has earned the authorization to operate (ATO) in the government cloud from 40+ separate federal departments and agencies. The company is FedRAMP-authorized and a certified service-disabled veteran-owned small business (SDVOSB).
To learn more, visit us online at www.intelliworxit.com. The company is active on social media sites, including LinkedIn and X.
Frank Strong
for Intelliworx
+1 202-352-5920
frank@swordandthescript.com
Visit us on social media:
LinkedIn
Facebook
X
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.